FROM CT IMAGE TO 3D MODEL
Thanks to new 3D imaging software, surgeons can now create physical models of their patients' inside
by Y. Ted Wu, Ph.D. (Published on Advanced Imaging, August 2001, pp. 20-23)
Mr. A. Waitz broke the radius of his right forearm in an automotive accident five years ago. It was poorly set initially and has been reset several times. He has been to some of the top surgeons in the US and had nine restorative surgeries so far. Because of the lack of good radiological information, the physicians were not able to achieve good alignment and hence the failure of all these surgeries. Multiple surgeries would result higher risk to the patient, as well as more costs and significant additional recovery times. In the case of nine surgeries with a typical minimum recovery time (length of time in a cast) of 6 weeks, it requires 54 weeks or more than a full year of time in recovery, as well as starting physical therapy again each time.
Surgery
today is still similar to what it did three thousand years ago: the
surgeons use their hands to directly control instruments and they use
their eyes to provide them with feedback about the effect of their
manipulations. The amount of information they have before a surgery is
critical to the success of the operation.
The developments in 3D imaging technology over the recent years have been focusing on the goals to not only let the physicians and surgeons to see better inside the body, but also create physical models from CT (Computed Tomography) and MRI (Magnetic Resonance Imaging). Using the model a surgeon is able to perform a "mock" surgery prior to ever entering the operating room. Some surgeons find that minutes or hours of operating time can be saved by careful preparation using the model.
Rendering a Surface Model
Able Software Corp. 3D-DOCTOR (Lexington, MA) is a 3D imaging software using vector-based surface model creation rather than raster-based systems to significantly improve computational efficiency and the quality of generated 3D models to be used by 3D printers and rapid prototyping machines.
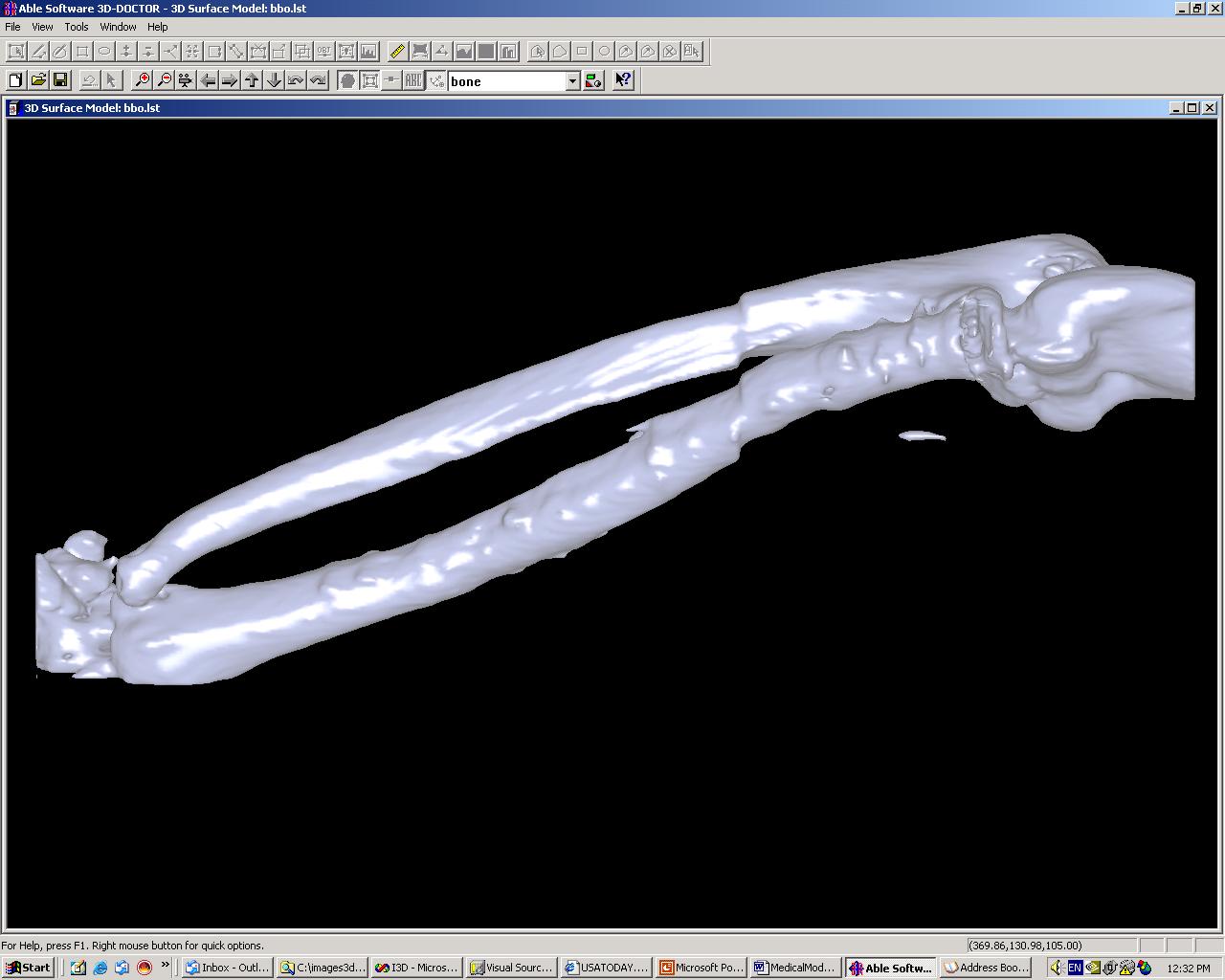
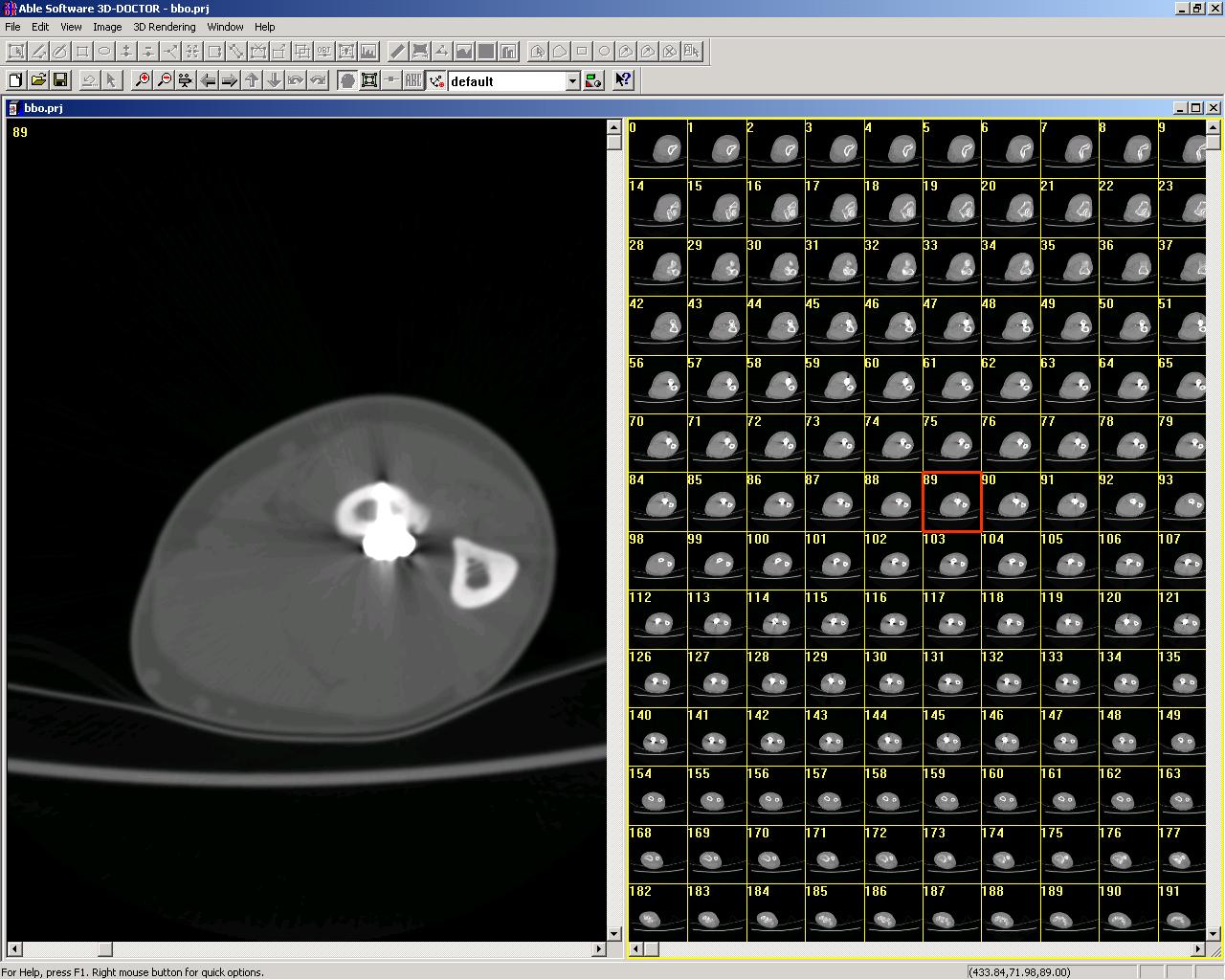
First, the image is segmented to isolate and trace the boundaries of the object of interest within the image set (Figure 1). A single CT or MRI image slice (512x512 16 bit) is about a half a megabyte in size and a typical CT/MRI image can have around 200 slices, which makes the total image size about 100 megabytes. Figure 2 shows a CT scan of a patient. Rather than work with all the pixel values as conventional 3D modeling systems do, 3D-DOCTOR defines the boundaries of objects in vectors -- a closed polygon with a given magnitude for all image slices. To create the 3D polygon based surface model, the surface rendering algorithm searches the best corresponding point in the neighbor slices to connect for forming surface triangles. When all boundary points are properly connected, a watertight surface model is created.
Thanks to the vector-based surface rendering algorithm, a 3D surface model can be created in a few seconds on a standard Pentium III class PC with 128 MB memory. The 3D volume rendering can be done in near real-time (from a few seconds to few minutes depending on the complexity of the object under study) without using any additional hardware accelerator. By comparison, other raster-based medical imaging software packages recommend workstations with dual P3’s and up to 1 GB of RAM, some of them have to use special volume rendering hardware for 3D volume display. The 3D surface model can be visualized on a PC in real time from any angle. The model can also be sliced or diced to show the image voxels on the model or at certain position within the body.
Creating The Physical Model
The 3D models are then saved to a file format that a 3D printer or a rapid prototyping machine accepts. For example, the STL (stereolithography) file format is commonly used on most 3D printers or rapid prototyping machines. Other standard formats include AutoCAD DXF, IGES and 3D Studio file formats.

A 3D printer takes the surface model and automatically creates a physical model using material such as resin, paper power or plastics. This process can take minutes to hours depending on the complexity of the model. Most 3D printers are still monochrome, using the same color as the material used. However, colors start to appear on some of the newer 3D printers and pretty soon multiple colors will be available for producing complex models.
Once the model is made, the surgeon not only can look it from any angle, but also touch it and even operate on it. Using the model a surgeon is able to perform a "mock" surgery prior to ever entering the operating room. Some surgeons find that minutes or hours of operating time can be saved by careful preparation using the model.
The model is a great tool for a surgeon to communicate with her patient about the upcoming procedure. Instead of looking at a textbook drawing or a generic anatomical model, the patient gets to visualize the procedure on their own model.
An added benefit is that the model becomes an ideal communication tool between surgeons and specialties on the case at hand. Unlike film or drawings, the model can only be interpreted basically one way, significantly reducing confusion or misunderstanding in the communication process.
Real-Life Applications
Doctors at the Massachusetts General Hospital Surgical Simulation Group (Boston, MA) are using 3D-DOCTOR to make replicas of real internal organs from CT images. Under a US Army grant, the group is combining a 3D surgical visualization with a life size mannequin of a human torso to create a “flight simulator for surgeons.” The system will be used to train US Army medical personnel on the best ways to handle penetrating battle wounds, such as insertion of tubing into the lungs to alleviate air pressure from gun wounds.
As for Mr. A. Waitz, he started his own searching for imaging tools to help his doctors better prepare and plan a surgery. He has found 3D-DOCTOR and is currently working with his doctors to use the software to create 3D models for both his left arm (normal) and the right arm (injured) to prepare another surgery. Hopefully with the help of the 3D imaging technologies and the real models, this will be the last surgery he’ll ever need--well, for this particular injury, at least.